The Effect of Childhood Trauma on Brain Development

The following studies highlight some of the effects of maltreatment on brain development:
Bremner, J. D., Southwick, S. M., & Charney, D. S. (1991, fall)
Bremner, J. D., Southwick, S. M., & Charney, D. S. (1991, fall). Animal Models for the Neurobiology of Trauma. National Center for PTSD Research Quarterly, 2(4), 1-7. (PDF Format – Acrobat Reader required)
Clinicians will notice parallels between the behavioral and biological sequelae of inescapable stress and the phe-nomenology of PTSD symptoms in their patients. The animal model of inescapable stress parallels the experience of being pinned down in combat or being the victim of repeated assaults. Inescapable stress produces a variety of behaviors in animals including abnormal alarm states, aggression, sensitivity to stress, altered sleep patterns, deficits in learning and memory, and withdrawal. These behaviors resemble those seen in patients with PTSD. For instance, evidence from animal findings of alterations in noradrenergic brain systems is consistent with emerging findings of abnormalities in noradrenergic systems in patients with PTSD as evidenced by abnormal responses to the alpha-2 noradrenergic receptor antagonist yohimbine. The identification of specific neurobiological abnormalities may lead to the development of new psychopharmacological and psychotherapeutic treatments based on the pathophysiology of PTSD.
Bremner JD, Randall P, et al. (1997)
Bremner, J. D. (1999)
Bremner, J. D. (1999). The Lasting Effects of Psychological Trauma on Memory and the Hippocampus.
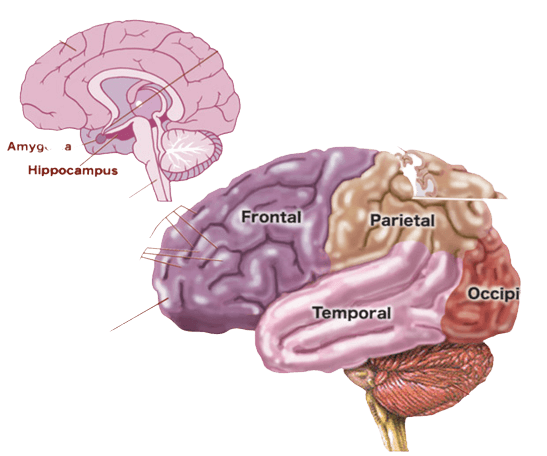
Childhood abuse and other extreme stressors can have lasting effects on brain areas involved in memory and emotion. The hippocampus is a brain area involved in learning and memory that is particularly sensitive to stress
Bremner, J. D. (2000)
Bremner, J. D. (2000). The Invisible Epidemic: Post-Traumatic Stress Disorder, Memory and the Brain. (PDF)
The biology of soul murder
The biology of soul murder: Fear can harm a child’s brain. Is it reversible? (Nov. 11, 1996). U.S. News & World Report
Excerpt: “Once viewed as genetically programmed, the brain is now known to be plastic, an organ molded by both genes and experience throughout life. A single traumatic experience can alter an adult’s brain: A horrifying battle, for instance, may induce the flashbacks, depression and hair-trigger response of post-traumatic stress disorder (PTSD). And researchers are finding that abuse and neglect early in life can have even more devastating consequences, tangling both the chemistry and the architecture of children’s brains and leaving them at risk for drug abuse, teen pregnancy and psychiatric problems later in life.”
Centers for Disease Control and Prevention (CDC). (2008)
Centers for Disease Control and Prevention (CDC). (2008). The Effects of Childhood Stress on Health Across the Lifespan
This booklet summarizes the research on childhood stress and its implications for adult health and well-being. Of particular interest is the stress caused by child abuse, neglect, and repeated exposure to intimate partner violence. Intensive and prolonged stress can lead to a variety of short- and long-term negative health effects. It can disrupt early brain development and compromise functioning of the nervous and immune systems. In addition, childhood stress can lead to health problems later in life including alcoholism, depression, eating disorders, heart disease, cancer, and other chronic diseases. This publication provides violence prevention practitioners with ideas about how to incorporate information on childhood stress into their work.
http://www.cdc.gov/ncipc/pub-res/pdf/Childhood_Stress.pdf (warning large file)
Chamberlain, D.B. (1989)
Chamberlain, D.B. (1989). Babies Remember Pain. Pre- and Peri-natal Psychology, 3(4), 297-310.
We are still enthralled by popular myths that babies don’t feel, don’t think, don’t remember, and have no sense of self. Scientific research shows these myths to be false and calls into question painful procedures and rituals at birth that are both inhumane and unnecessary.
Dannlowski et al. (2012)
Dannlowski et al. (2012). Limbic Scars: Long-Term Consequences of Childhood Maltreatment Revealed by Functional and Structural Magnetic Resonance Imaging. Biological Psychiatry, 71(4), 286-293.
Childhood maltreatment is associated with remarkable functional and structural changes even decades later in adulthood. These changes strongly resemble findings described in depression and PTSD. Therefore, the present results might suggest that limbic hyperresponsiveness and reduced hippocampal volumes could be mediators between the experiences of adversities during childhood and the development of emotional disorders.
De Bellis, Michael D. (1999)
De Bellis, Michael D. (1999). Developmental Traumatology: Neurobiological Development in Maltreated Children With PTSD. Psychiatric Times, 16 (11),
Science shows that child abuse may be associated with alterations of the body’s major stress systems. These neurobiological effects may cause delays or deficits in a child’s ability to achieve age-appropriate behavioral, cognitive and emotional regulation.
De Bellis, M. D., Chrousos, G. P., Dorn, L. D
De Bellis, M. D., Chrousos, G. P., Dorn, L. D., Burke, L., Helmers, K., Kling, M. A., Trickett, P. K., & Putnam, F. W. (1994). Hypothalamic-pituitary-adrenal axis dysregulation in sexually abused girls. Journal of Clinical Endocrinology & Metabolism, 78(2), 249-55.
Childhood sexual abuse is associated with an increased incidence of age-concurrent and adult psychopathology. Little is known, however, about the biological manifestations and sequelae of childhood sexual abuse. In this study, we characterized the hypothalamic-pituitary-adrenal axis of a self-selected sample of sexually abused and control girls recruited from a prospective longitudinal study. Plasma ACTH and total and free cortisol responses to ovine CRH (oCRH) stimulation were measured in 13 sexually abused and 13 control girls, aged 7-15 yr. Psychiatric profiles and 24-h urinary free cortisol (UFC) measures were also obtained. Sexually abused girls had a greater incidence of suicidal ideation (chi 2 = 4.51; df = 1; P < 0.05), suicide attempts (chi 2 = 4.51; df = 1; P < 0.05), and dysthymia (chi 2 = 8.85; df = 1; P < 0.01) than control girls. Sexually abused girls showed significantly lower basal (t = 2.1; df = 24; P < 0.05), and net oCRH stimulated (t = 2.2; df = 24; P < 0.05) ACTH levels and significantly reduced total ACTH responses (t = 2.5; df = 24; P < 0.05) compared with control subjects. Their total and free basal and oCRH-stimulated plasma cortisol levels and 24-h UFC measures, however, were similar to those in controls. The attenuated plasma ACTH with corresponding robust plasma cortisol responses to oCRH stimulation and normal 24-h UFC measures in sexually abused girls suggest a dysregulatory disorder of the HPA axis in these individuals. This may reflect pituitary hyporesponsiveness to oCRH. The ability of sexually abused subjects to correct for the proposed pituitary hyporesponsiveness to CRH may be related to their young age and the presence of intact glucocorticoid feedback regulatory mechanisms.
DeBellis, M.D., Keshavan, M.S., Clark, D.B.
DeBellis, M.D., Keshavan, M.S., Clark, D.B., Casey, B.J., Giedd, J.N., Boring, A.M., Frustaci, K. & Ryan, N.D. (1999). Pituitary-Adrenal and Autonomic Responses to Stress in Women After Sexual and Physical Abuse in Childhood Developmental traumatology part II: Brain development. Society of Biological Psychiatry, 45, 1271-1284.
PTSD subjects had smaller intracranial and cerebral volumes than matched controls. The total midsagittal area of corpus callosum and middle and posterior regions remained smaller; while right, left, and total lateral ventricles were proportionally larger than controls, after adjustment for intracranial volume. Brain volume robustly and positively correlated with age of onset of PTSD trauma and negatively correlated with duration of abuse. Symptoms of intrusive thoughts, avoidance, hyperarousal or dissociation correlated positively with ventricular volume, and negatively with brain volume and total corpus callosum and regional measures. Significant gender by diagnosis effect revealed greater corpus callosum area reduction in maltreated males with PTSD and a trend for greater cerebral volume reduction than maltreated females with PTSD. The predicted decrease in hippocampal volume seen in adult PTSD was not seen in these subjects.
CONCLUSIONS: These data suggest that the overwhelming stress of maltreatment experiences in childhood is associated with adverse brain development.
De-Bellis, M. D., Lefter, L., Trickett, P. K., & Putnam
De-Bellis, M. D., Lefter, L., Trickett, P. K., & Putnam, F. W. Urinary catecholamine excretion in sexually abused girls. (1994). Journal of the American Academy of Child and Adolescent Psychiatry , 33 (3), 320-27.
This study measured urinary catecholamine and metabolite concentrations of nine stress-related hormones in 12 sexually abused and 9 control girls (age 8 to 15 years). Psychiatric profiles also were obtained. The abused girls excreted significantly greater amounts of stress-related hormones (e.g., metanephrine, vanillylmandelic acid, homovanillic acid, and total catecholamine synthesis as measured by the sum of epinephrine, norepinephrine, dopamine, and their metabolites) as compared with controls. Sexually abused girls also had a greater incidence of suicidal ideation, suicide attempts, and dysthymia than did controls. The findings are clinically significant in their similarity to the psychobiology of both post-traumatic stress disorder and major depressive disorder.
Driessen, M., Herrmann, J., Stahl, K., et al. (2000)
Driessen, M., Herrmann, J., Stahl, K., et al. (2000). Magnetic resonance imaging volumes of the hippocampus and the amygdala in women with borderline personality disorder and early traumatization. Arch Gen Psychiatry, 5 7, 1115-1122
ABSTRACT: Background: Based on findings of stress-induced neural disturbances in animals and smaller hippocampal volumes in humans with posttraumatic stress disorder), we hypothesized that patients with borderline personality disorders (BPD), who often are victims of early traumatization, have smaller volumes of the hippocampus and the amygdala. We assumed that volumes of these brain regions are negatively correlated with traumatic experiences and with neuropsychological deficits.
Methods: We studied 21 female patients with BPD and a similar group of healthy controls. We performed clinical assessments, a modified version of the Childhood Trauma Questionnaire, and magnetic resonance imaging volumetric measurements of the hippocampus, amygdala, temporal lobes, and prosencephalon. Neuropsychological testing included scales on which disturbances in BPD were previously reported.
Results: The patients with BPD had nearly 16% smaller volumes of the hippocampus (P<.001) and 8% smaller volumes of the amygdala (P<.05) than the healthy controls. The results for both hemispheres were nearly identical and were controlled for the volume of the prosencephalon and for head tilts. The volumes of the hippocampus were negatively correlated with the extent and the duration of self-reported early traumatization only when BPD and control subjects were considered together. Levels of neuropsychological functioning were associated with the severity of depression but not with the volumes of the hippocampus.
Conclusion: In female patients with BPD, we found reduction of the volumes of the hippocampus (and perhaps of the amygdala), but the association of volume reduction and traumatic experiences remains unclear.
Gaensbauer T. J. (1995)
Gaensbauer T. J. (1995). Trauma in the preverbal period. Symptoms, memories, and developmental impact. Psychoanalytic Study of the Child , 50 , 122-49.
This article describes five children who experienced traumas during the preverbal period. The clinical presentations are oriented around three questions:
- What are the expectable symptomatic reactions of preverbal infants to trauma?
- To what extent and in what forms are preverbal traumatic experiences retained in memory?
- Does trauma in the preverbal period have endurng effects?
The traumas were all relatively circumscribed and predominantly physical in nature. At the time of their traumas, the children ranged in age from 7 to 15 months. None of them had achieved verbal fluency beyond single words. The amount of time that had elapsed from the point of the traumas to the author’s initial contact with the children ranged from 1 to 7 years. The author attempted to document other factors that might be contributing to the children’s behavior and symptoms including communications with their parents about the trauma. The ways in which the children reenacted their traumas, the contexts in which the material emerged, the associated affects and symptomatology, and the defensive operations brought into play, all suggested that the primary source of the child’s communications was internalized personal experience rather than declarative knowledge obtained from outside sources.
The material presented indicates that even prior to the onset of language fluency, symptomatology consistent with traditional post-traumatic diagnostic criteria can be observed. These cases suggest that the capacity to encode and retain meaningful internal representations of the salient elements of a traumatic experience may be present as early 7 months of age and do not depend on the achievement of language fluency. The developmental implications of early trauma, particularly if it is severe, appear to be significant.
Gurvits, T. V, Gilbertson
Gurvits, T. V, Gilbertson, M. W., Lasko, N. B., Orr, S. P., & Pitman, R. K. (1997). Neurological status of combat veterans and adult survivors of sexual abuse PTSD. Annals of the New York Academy of Sciences, 821 , 468-71.
ABSTRACT: So-called “soft” neurological signs (NSS) have been used as an instrument for investigation of organic brain dysfunction in psychiatric disorders including schizophrenia and obsessive-compulsive disorder. NSS are generally considered to reflect immaturities in development of language, motor coordination, or perception. We previously demonstrated a statistically significant increase of NSS in Vietnam combat veterans with PTSD. Using a more precise methodology, the present study examines NSS in PTSD and non-PTSD participants and explores the hypothesis that participants with PTSD will have greater neurological impairment and compromised developmental history in independent samples in which the nature of the traumatic experience and gender differs. This study examined two groups of traumatized individuals, male Vietnam combat veterans and adult female survivors of childhood sexual abuse.
Gurvits TV, Gilbertson MW, Lasko NB
Gurvits TV, Gilbertson MW, Lasko NB, Tarhan AS, Simeon D, Macklin ML, Orr SP, & Pitman RK. (2000). Neurologic soft signs in chronic posttraumatic stress disorder. Archives of General Psychiatry, 57(2), 181-6.
ABSTRACT: Background: Subtle neurologic impairment has been reported in several mental disorders. The goals of the present study were to evaluate neurologic status in patients of both sexes with chronic posttraumatic stress disorder (PTSD) from different traumatic experiences.
Methods: Twenty-one adult women who were sexually abused as children (12 with PTSD, 9 without) and 38 male Vietnam War combat veterans (23 with PTSD, 15 without) underwent examination for 41 neurologic soft signs, which were scored by the examiner as well as a blind rater observing videotapes. Subject history was obtained with special attention to neurodevelopmental problems. Psychometrics included the Wender Utah Rating Scale for symptoms of childhood attention-deficit/hyperactivity disorder and the Michigan Alcoholism Screening Test. Veterans also completed the Combat Exposure Scale and subtests of the Wechsler Adult Intelligence Scale-Revised.
Results: Average neurologic soft sign scores (interrater reliability = 0.74) of women with PTSD owing to sexual abuse in childhood (mean [SD], 0.77 [0.32]) and veteran men (0.72 [0.20]) with combat-related PTSD were comparable and significantly (P<.001) higher than those of women sexually abused as children (0.42 [0.10]) and combat veteran men (0.43 [0.17]) without PTSD. This effect could not be explained by a history of alcoholism or head injury. Subjects with PTSD reported more neurodevelopmental problems and more childhood attention-deficit/hyperactivity disorder symptoms and had lower IQs, all of which were significantly correlated with neurologic soft signs.
Conclusion: Neurologic compromise is evident from subject history and findings from physical examination in both women and men with chronic PTSD who had experienced different kinds of traumatic events in childhood and adulthood.
Hart, J., Gunnar, M. & Cicchetti, D. (1995)
Heim, C., Newport, D. J., Heit, S., Graham, Y. P.
Heim, C., Newport, D. J., Heit, S., Graham, Y. P., Wilcox, M., Bonsall, R., Miller, A. H., & Nemeroff, C. B. (2000, August 2). Pituitary-Adrenal and Autonomic Responses to Stress in Women After Sexual and Physical Abuse in Childhood . Journal of the American Medical Association , 284(5), 592-7.
When exposed to stress, abused women with and without current major depression exhibited increased ACTH concentrations compared with controls and nonabused depressed women. Women with histories childhood trauma were found to exhibit a counterregulatory adaptation of the adrenal cortex as reflected by increased ACTH concentrations but normal cortisol responses. Similar results have been observed in some animal models of severe early stress. It is concluded that severe stress early in life is associated with persistent sensitization of the pituitary-adrenal and autonomic stress response, which, in turn, is likely related to an increased risk for adulthood development of mood and anxiety disorders. The authors state that: “This is the first human study to report persistent changes in stress reactivity in adult survivors of early trauma.”
Heim, C., Newport, D. J., Bonsall, R., Miller, A. H.
Heim, C., Newport, D. J., Bonsall, R., Miller, A. H., & Nemeroff, C. B. (2001). Altered Pituitary-Adrenal Axis Responses to Provocative Challenge Tests in Adult Survivors of Childhood Abuse. American Journal of Psychiatry, 158, 575-581.
Abstract: OBJECTIVE: Early adverse life events may predispose individuals to the development of mood and anxiety disorders in adulthood, perhaps by inducing persistent changes in corticotropin-releasing factor (CRF) neuronal systems. The present study sought to evaluate pituitary-adrenal responses to standard hypothalamic-pituitary-adrenal axis challenge tests in adult female survivors of childhood abuse with and without major depressive disorder.
METHOD: Plasma ACTH and cortisol responses to the administration of 1 µg/kg ovine CRF and plasma cortisol responses to the administration of 250 µg ACTH 1-24 were measured in healthy women without early life stress (N=20), women with childhood abuse without major depressive disorder (N=20), women with childhood abuse and major depressive disorder (N=15), and women with major depression but no early life stress (N=11).
RESULTS: Abused women without major depressive disorder exhibited greater than usual ACTH responses to CRF administration, whereas abused women with major depressive disorder and depressed women without early life stress demonstrated blunted ACTH responses. In the ACTH 1-24 stimulation test, abused women without major depressive disorder exhibited lower baseline and stimulated plasma cortisol concentrations. Abused women with comorbid depression more often suffered from posttraumatic stress disorder and reported more recent life stress than abused women without major depressive disorder.
CONCLUSIONS: These findings suggest sensitization of the anterior pituitary and counterregulative adaptation of the adrenal cortex in abused women without major depressive disorder. On subsequent stress exposure, women with a history of childhood abuse may hypersecrete CRF, resulting in down-regulation of adenohypophyseal CRF receptors and symptoms of depression and anxiety.
Ito, Y., Teicher, M. H., Glod, C. A
Ito, Y., Teicher, M. H., Glod, C. A., Harper, E. M., et al. (1993). Increased prevalence of electrophysiological abnormalities in children with psychological, physical and sexual abuse. Journal of Neuropsychiatry and Clinical Neurosciences , 5(4), 401-8.
The aim of the present study was to ascertain whether childhood physical, sexual, or psychological abuse was associated with direct evidence of neurobiological abnormalities in 104 patients (mean age of 13 years) admitted to an inpatient unit. Subjects were given a neurological examination, neuropsychological testing, EEG, brain electrical activity mapping, computerized tomography (CT) scans, and magnetic resonance imaging (MRI). Patients with evidence of a preexisting neurological abnormality were not included in the study. Increased electrophysiological abnormalities were found in subjects with a history of abuse compared with nonabused subjects. Abnormalities occurred predominantly in the left side of the frontal, temporal, or anterior regions for physically and/or sexually abuse subjects. Children who had been psychologically abused or neglected but not physically or sexually abused were found to have abnormalities in the left side of the temporal region only. Data may support the hypothesis that early abuse alters brain development, particularly limbic structures. It is postulated that left hemisphere dysfunction in children may result in greater use or dependence on the right hemisphere. Increased dependence on the right frontal lobes may, in turn, lead to increased perception and expression of negative emotion and may facilitate unconscious storage of painful childhood memories.
Ito, Y., Teicher, M. H., Glod, C. A
Ito, Y., Teicher, M. H., Glod, C. A., & Ackerman, E. (1998). Preliminary evidence for aberrant cortical development in abused children: A quantitative EEG study. Journal of Neuropsychiatry & Clinical Neurosciences, 10, 298-307.
The objectives of this study were to investigate cortical development and hemispheric asymmetry in abused children. Fifteen hospitalized children (mean age 10.7 +/- 2.5 years) with severe physical or sexual abuse and 15 normal children (10.1 +/- 3.1 years) were studied with quantitative EEG. Abused children had higher levels of left hemisphere coherence and a reversed asymmetry, with left hemisphere coherence significantly exceeding right hemisphere coherence. Left hemisphere coherence decreased more rapidly across electrode distance in normal subjects, suggesting that increased left coherence in abused patients stemmed from a deficit in left cortical differentiation. These findings support the hypothesis that early severe abuse may have a deleterious effect on brain development.
Ladd, C.O. et al, (2000)
Lemieux, A. M., & Coe, C. I. (1995)
Lemieux, A. M., & Coe, C. I. (1995). Abuse-related posttraumtic stress disorder: Evidence for chronic neuroendocrine activation in women. Psychosomatic Medicine, 57(1), 105-15.
(Adapted from text): This study examined whether women with PTSD related to childhood sexual abuse (CSA) would display elevated norepinephrine-to-cortisol ratios similar to that found in combat veterans diagnosed with PTSD. Subjects were three groups of women: (1) 11 women who experienced CSA diagnosed with PTSD; (2) 8 women who experienced CSA, but were not currently diagnosed with PTSD; and (3) 7 age-comparable women who had not experienced CSA and were not currently in psychotherapy (controls). All subjects were asksed to complete various measures of PTSD symptoms, general physical heath status and premenstrual symptoms. In addition 24-urinary catecholamines timed with the menstrual cycle, creatinine levels, and urinary-free cortisol levels were obtained.
The results verify that abuse-related PTSD is accompanied by neuroendocrine activation as well as significant psychological disturbance. The abuse-related PTSD group had significantly evelated daily levels of norepinephrine, epinephrine, dopamine, and cortisol even after adjusting for creatinine clearance rates. Because of the parallel elevation in cortisol, the norepinephrine-to-cortisol ration was not significantly elevated in the PTSD diagnosed women as has been shown in male combat veterans with PTSD. It is possible that this discrepancy may reflect an important gender different, an interaction between gender and age at onset of the traumatic experience (childhood versus adulthood), or physicalogical variation related to the phase of the disorder. Both groups of abused women also reported a higher incidence of premenstrual symptoms than the controls.
The researchers also investigated several findings suggested by previous studies–polyuria (excess production of urine) and obesity. The PTSD-positive group showed a tendency toward obesity that was nearly twice the national average. In addition, both abused groups regardless of PTSD status showed a tendency for polyuria (the mean dialy output of urine was 2231 ml in PTSD+ subjects, 1759 ml in PTSD- subjects, and 1192 ml in the controls). It is suggested that the finding of polyuria may have revealed an important physiological biomarker in this population. The elevated urine volume found in the abused patients may reflect high levels of liquid consumption, a pattern that has been documented in both psychotic patients and manic depressive patients.
McCrory, E., De Brito, S. A., & Viding, E.(2011)
McCrory, E., De Brito, S. A., & Viding, E.(2011). The impact of childhood maltreatment: A review of neurobiological and genetic factors. Frontiers in Psychiatry. 2:48. Epub 2011 Jul 28.
Provides a brief overview of neuroendocrine findings, which indicate an association between maltreatment and atypical development of the hypothalamic–pituitary–adrenal axis stress response, which may predispose to psychiatric vulnerability in adulthood. Then reviews the magnetic resonance imaging (MRI) studies that have investigated possible structural and functional brain differences in children and adults who have experienced childhood maltreatment. Differences in the corpus callosum identified by structural MRI have now been reliably reported in children who have experienced abuse, while differences in the hippocampus have been reported in adults with childhood histories of maltreatment. In addition, there is preliminary evidence from functional MRI studies of adults who have experienced childhood maltreatment of amygdala hyperactivity and atypical activation of frontal regions. These functional differences can be partly understood in the context of the information biases observed in event-related potential and behavioral studies of physically abused children. Then discusses research that has indicated that the effect of environmental adversity may be moderated by genotype, reviewing pertinent studies pointing to gene by environment interactions.
McGowan, P. O., Sasaki, A., Huang, T. C. T., Unterberger, A
McGowan, P. O., Sasaki, A., Huang, T. C. T., Unterberger, A., Suderman, M., Ernst, C., et al. (2008). Promoter-Wide Hypermethylation of the Ribosomal RNA Gene Promoter in the Suicide Brain. PLoS ONE, 3(5), e2085.
This landmark study shows how environment affects genes in brains of men who killed themselves. A team of McGill University scientists has discovered important differences between the brains of suicide victims who experienced abuse as children and the brains of nonabused adults. Although the genetic sequence was identical in the suicide and non-suicide brains, there were differences in their epigenetic marking – a chemical coating influenced by environmental factors. The researchers examined a set of genes that code for rRNA, a basic component of the machinery that creates protein in cells. Protein synthesis is critical for learning, memory and the building of new connections in the brain; it can affect decision-making and other behaviour.
Mehta, M. A., Golembo, N. I., Nosarti, C., Colvert, E., Mota
Mehta, M. A., Golembo, N. I., Nosarti, C., Colvert, E., Mota, A., Williams, S. C., Rutter, M., & Sonuga-Barke, E. J. (2009). Amygdala, hippocampal and corpus callosum size following severe early institutional deprivation: The English and Romanian Adoptees study pilot. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 50, 943-951.
The adoption into the UK of children who have been reared in severely deprived conditions provides an opportunity to study possible association between very early negative experiences and subsequent brain development. This cross-sectional study was a pilot for a planned larger study quantifying the effects of early deprivation on later brain structure. We used magnetic resonance imaging (MRI) to measure the sizes of three key brain regions hypothesized to be sensitive to early adverse experiences. Our sample was a group of adoptee adolescents (N = 14) who had experienced severe early institutional deprivation in Romania and a group of non-institutionalised controls (N = 11). The total grey and white matter volumes were significantly smaller in the institutionalised group compared with a group of non-deprived, non-adopted UK controls. After correcting for difference in brain volume, the institutionalised group had greater amygdala volumes, especially on the right, but no differences were observed in hippocampal volume or corpus callosum mid-sagittal area. The left amygdala volume was also related to the time spent in institutions, with those experiencing longer periods of deprivation having a smaller left amygdala volume. These pilot findings highlight the need for future studies to confirm the sensitivity of the amygdala to early deprivation
Perry, B. D.
Perry, B. D. (1994). Neurobiological Sequelae of Childhood Trauma: Post traumatic Stress Disorders in Children. In Catecholamine Function in Post Traumatic Stress Disorder: Emerging Concepts (M Murburg, Ed.) American Psychiatric Press, Washington, DC, 253-276.
Abstract: The present chapter will review childhood PTSD with specific focus on neurobiological sequelae of childhood trauma and present some preliminary evidence of altered functioning of brainstem catecholamine systems in childhood PTSD. In specific, it is hypothesized that the abnormal patterns of catecholamine activity associated with prolonged ‘alarm reactions’ induced by traumatic events during infancy and childhood can result in altered development of the central nervous system (CNS). Furthermore, it is hypothesized that this altered development includes a ‘dysregulated’ brainstem which in turn results in a host of signs and symptoms related to abnormal brainstem functioning, including altered cardiovascular regulation, affective lability, behavioral impulsivity, increased anxiety, increased startle response and sleep abnormalities. Finally, early life experience is discussed, in context of childhood trauma, as an ‘expresser of genetic predispositions.
Perry, B. D. (1996). Neurodevelopmental Adaptations to Violence: How Children Survive the Intragenerational Vortex of Violence. In Violence and Childhood Trauma: Understanding and Responding to the Effects of Violence on Young Children. Cleveland, Ohio: Gund Foundation Publishers, pp.67-80.
Perry, B. D. (1997). Incubated in Terror: Neurodevelopmental Factors in the “Cycle of Violence.” In J. Osofsky (Ed.). Children, Youth and Violence: The Search for Solutions . (pp. 124-148). New York: Guilford Press.
How violence alters the brain and nervous system of the developing child.
Perry, B. D. (1997). Altered Brain Development Following Global Neglect in Early Childhood. (1997). Academy version of a paper presented at the Society for Neuroscience Annual Meeting, New Orleans.
Perry, B. D. (1998). Neurophysiological Aspects of Anxiety Disorders in Children. In: Textbook of Pediatric Neuropsychiatry. In C.E. Coffey & R.A. Brumback (Eds.), Textbook of Pediatric Neuropsychiatry. (pp. 579-594). Washington, D.C: American Psychiatric Press, Inc.
Perry, B.D. (1999). Memories of fear: How the Brain Stores and Retrieves Physiologic States, Feelings, Behaviors and Thoughts from Traumatic Events. In J.M. Goodwin & R. Attias (Eds.), Splintered Reflections: Images of the Body In Trauma. (pp. 9-38). New York: Basic Books.
Perry, B.D. (1999). Violence and Childhood: How Persisting Fear Can Alter the Developing Child’s Brain.
Perry, B. D. (2000). Traumatized children: How childhood trauma influences brain development. The Journal of the California Alliance for the Mentally Ill 11(1), 48-51.
Perry, B.D. (2001). The neurodevelopmental impact of violence in childhood. In D. Schetky & E. Benedek (Eds.), Textbook of Child and Adolescent Forensic Psychiatry. Washington, D.C.: American Psychiatric Press, Inc.
Perry, B.D. (2001) The neuroarcheology of childhood maltreatment: The neurodevelopmental costs of adverse childhood events. In B. Geffner (Ed.), The Cost of Child Maltreatment: Who Pays? We All Do. San Diego, CA: Family Violence & Sexual Assault Institute.
Perry, B.D. (2001). Trauma and Terror in Childhood: The Neuropsychiatric Impact of Childhood Trauma. In Ed., I. Schulz, S. Carella & D.O. Brady (Eds.). Handbook of Psychological Injuries: Evaluation, Treatment and Compensable Damages. American Bar Association Publishing.
Perry, B.D. (2002). Childhood Experience and the Expression of Genetic Potential: What Childhood Neglect Tells Us About Nature and Nurture. Brain and Mind, 3, 79-100,
Abstract.
Studies of childhood abuse and neglect have important lessons for considerations of nature and nurture. While each child has unique genetic potentials, both human and animal studies point to important needs that every child has, and severe long-term consequences for brain function if those needs are not met. The effects of the childhood environment, favorable or unfavorable, interact with all the processes of neurodevelopment (neurogenesis, migration, differentiation, apoptosis, arborization, synaptogenesis, synaptic sculpting, and myelination). The time courses of all these neural processes are reviewed here along with statements of core principles for both genetic and environmental influences on all of these processes. Evidence is presented that development of synaptic pathways tends to be a “use it or lose it” proposition. Abuse studies from the author’s laboratory, studies of children in orphanages who lacked emotional contact, and a large number of animal deprivation and enrichment studies point to the need for children and young nonhuman mammals to have both stable emotional attachments with and touch from primary adult caregivers, and spontaneous interactions with peers. If these connections are lacking, brain development both of caring behavior and cognitive capacities is damaged in a lasting fashion. These effects of experience on the brain imply that effects of modern technology can be positive but need to be monitored. While technology has raised opportunities for children to become economically secure and literate, more recent inadvertent impacts of technology have spawned declines in extended families, family meals, and spontaneous peer interactions. The latter changes have deprived many children of experiences that promote positive growth of the cognitive and caring potentials of their developing brains.
Perry, B.D. (in press). Sexual Abuse of Infants. A five-part question focusing on sexual abuse during infancy
Perry, B. D., Conroy, L., & Ravitz, A. (1991). Persisting psychophysiological effects of traumatic stress: The memory of “states“. Violence Update, 1(8), 1-11.
Perry, B. D., & Marcellus, J. E. (1997). The Impact of Abuse and Neglect on the Developing Brain. Colleagues for Children, 7, 1-4. [Missouri Chapter of the National Committee to Prevent Child Abuse]
Perry, B. D., & Pollard, R. Altered brain development following global neglect in early childhood. Society For Neuroscience: Proceedings from Annual Meeting , New Orleans, 1997)
Perry, B.D., & Pollard, R. (1998). Homeostasis, stress, trauma, and adaptation: A neurodevelopmental view of childhood trauma. Child and Adolescent Psychiatric Clinics of North America , 7, 33-51.
This chapter discusses the impact of traumatic experiences on the development and functioning of children as viewed through the lens of developmental neurobiology. The recurring theme in a neurodevelopmental view is the remarkable malleability of the developing brain. Dr. Perry shows how the brain’s exquisite sensitivity to experience in early childhood allows traumatic experiences during infancy and childhood to impact all future emotional, behavioral, cognitive, social and physiological functioning.
Perry, B.D., Pollard, R.A., Blakley, T.L., Baker, W.L., & Vigilante, D. (1995). Childhood trauma, the neurobiology of adaptation and use-dependent development of the brain: How states become traits. Infant Mental Health Journal, 16, 271-291.
Perry, B. D., Southwick, S. W., Yehuda, R., & Giller, E. L. (1990). Adrenergic receptor regulation in post-traumatic stress disorder. In Advances in Psychiatry: Biological Assessment and Treatment of Post Traumatic Stress Disorder (E. L. Giller , Ed.). American Psychiatric Press, Washington, DC, 87-115.
Pitman, R. & Orr, S
Porges, S. (2001)
Rosler, A. (1994). Long-term effects of childhood
Schore, A. ( 1999)
Schore, A. N. (2001)
Schore, A. N. (2001). The Effects of a Secure Attachment Relationship on Right Brain Development, Affect Regulation, and Infant Mental Health. Infant Journal of Mental Health, 22, 7-66.
Abstract: Over the last ten years the basic knowledge of brain structure and function has vastly expanded, and its incorporation into the developmental sciences is now allowing for more complex and heuristic models of human infancy. In a continuation of this effort, in this two part work I integrate current interdisciplinary data from attachment studies on dyadic affective communications, neuroscience on the early developing right brain, psychophysiology on stress systems, and psychiatry on psychopathogenesis in order to provide a deeper understanding of the psychoneurobiological mechanisms that underlie infant mental health.
In this paper I detail the neurobiology of a secure attachment, an exemplar of adaptive infant mental health, and focus upon the primary caregiver’s psychobiological regulation of the infant’s maturing limbic system, the brain areas specialized for adapting to a rapidly changing environment. The infant’s early developing right hemisphere has deep connections into the limbic and autonomic nervous systems and is dominant for the human stress response, and in this manner the attachment relationship facilitates the expansion of the child’s coping capacities. This model suggests that adaptive infant mental health can be fundamentally defined as the earliest expression of flexible strategies for coping with the novelty and stress that is inherent in human interactions. This efficient right brain function is a resilience factor for optimal development over the later stages of the life cycle.
Schore, A. N. (2001)
Schore, A. N. (2001). The Effects of Early Relational Trauma on Right Brain Development, Affect Regulation, and Infant Mental Health. Infant Journal of Mental Health, 22, 201-269.
Abstract: A primary interest of the field of infant mental health is in the early conditions that place infants at risk for less than optimal development. The fundamental problem of what constitutes normal and abnormal development is now a focus of developmental psychology, infant psychiatry, and developmental neuroscience. In the second part of this sequential work, I present interdisciplinary data to more deeply forge the theoretical links between severe attachment failures, impairments of the early development of the right brain’s stress coping systems, and maladaptive infant mental health.
In the following I offer thoughts on the negative impact of traumatic attachments on brain development and infant mental health, the neurobiology of infant trauma, the neuropsychology of a disorganized / disoriented attachment pattern associated with abuse and neglect, trauma-induced impairments of a regulatory system in the orbitofrontal cortex, the links between orbitofrontal dysfunction and a predisposition to posttraumatic stress disorders, the neurobiology of the dissociative defense, the etiology of dissociation and body-mind psychopathology, the effects of early relational trauma on enduring right hemispheric function, and some implications for models of early intervention. These findings suggest direct connections between traumatic attachment, inefficient right brain regulatory functions, and both maladaptive infant and adult mental health.
Siegel, D. (1999)
Siegel, D. (1999). The Developing Mind. Guilford Press, New York.
Siegel, D. J. (2001)
Siegel, D. J. (2001). Toward an Interpersonal Neurobiology of the Developing Mind: Attachment relationships, “mindsight,” and neural integration. Infant Mental Health Journal, Special Edition on Contributions of the Decade of the Brain to Infant Psychiatry, 22, 67-94.
Abstract: This article reviews findings from a wide range of scientific disciplines in exploring the idea that the mind develops at the interface between human relationships and the unfolding structure and function of the brain. Recent discoveries from a number of independent fields, including those of developmental psychology and cognitive neuroscience, can be synthesized into an integrated framework for understanding how the brain gives rise to mental processes and is directly shaped by interpersonal experiences. This “interpersonal neurobiology” (Siegel, 1999) presents an integrated view of how human development occurs within a social world in transaction with the functions of the brain that give rise to the mind. This framework suggests some basic principles for conceptualizing the essential experiential ingredients that may facilitate the development of the mind, emotional well-being, and psychological resilience during early childhood and perhaps throughout the lifespan. At the core of these processes is a fundamental mechanism of integration which can be seen at a variety of levels, from the interpersonal to the neurological. Integration may be conceptualized as the basic process that secure attachments facilitate in promoting psychological well-being. This article will summarize these concepts and offer some ideas about their implications for practice and future investigations.
Stein, M. B., Koverola, C., Hanna
Stein, M. B., Koverola, C., Hanna, C., Torchia, M. G., & McClarty, B. (1997). Hippocampal volume in women victimized by childhood sexual abuse. Psychological Medicine , 27(4), 951-9.
Numerous studies have determined that exposure to childhood sexual abuse (CSA) is a risk factor for the subsequent development of adult psychopathology, however, only recently have researchers considered the possibility that severe emotional trauma may affect not only the psyche but the brain. This study examined verbal explicit memory functioning and hippocampal volume 21 adult females who reported have experienced severe CSA and 21 adult females who had no history of any type of childhood trauma. The researchers hypothesized that the CSA subjects would have smaller hippocampi than nonabused subjects and that verbal explicit memory functioning and hippocampal volume would be negatively correlated in abused subjects.
Subjects were recruited using notices posted in waiting rooms in several community women’s health care clinics. Subjects were ruled ineligible if they had a history of significant medical illness or neurological conditions. Subjects currently abusing alcohol or other substances were also excluded. All subjects were evaluated using a version of the Structured clinical Interview for DSM-IV (SCID) and a separate interview for DSM-IV Dissociative Disorders (SCID-D). Subjects were also administered the Dissociative Experiences Scale (DES) and the Beck Depression Inventory (BDI). The Clinician-Administered PTSD Scale (CAPS) was used to assess PTSD severity in the abuse victims. To assess intellectual functioning, subjects were administered 5 subtests of the Weschler Adult Intelligence Scale-Revised (WAIS-R). Explicit memory performance was assessed using the California Verbal Learning Test (CVLT).
The two groups of women were similar on all indices of sociodemographic status, body morphometrics, and intellectual functioning. Results indicated that women reporting CSA had lower hippocampal volumes—particularly on the left side—compared to comparable women without abuse histories. Within the CSA subjects, the severity of dissociative and, to a lesser extent, other PTSD symptoms correlated significantly with left hippocampal volume. These findings support a possible relationship between hippocampal dysfunction and post-traumatic psychiatric symptoms. There were no significant differences between groups on explicit memory functioning and no correlations were found between hippocampal volume and any of the measures of learning and memory.
The authors note that while it is possible that abuse experiences result in hippocampal atrophy, an alternative hypothesis which deserves consideration is that the hippocampal differences might have been present prior to the trauma, and that such differences might predispose the individual to the development of PTSD in the face of exposure to psychological trauma.
Schwarz, E., & Perry, B. D. (1994)
Schwarz, E., & Perry, B. D. (1994). The post-traumatic response in children and adolescents. Psychiatric Clinics of North America, 17(2), 311-326.
Each year in the United States over 3 million children and adolescents experience some form of traumatic event. The adaptive and maladaptive responses to trauma in children and adolescents is compared with adults. Post-traumatic disorders are viewed as the maladaptive persistence of a previously adaptive set of mental and physiological responses to the trauma organized as ‘malignant memories’. This view allows integration of neurodevelopmental and psychosocial conceptualizations that underlie rational clinical assessment and treatment.
Teicher, M.D. (2000)
Teicher, M.D. (2000). Wounds that time won’t heal: The neurobiology of child abuse. Cerebrum: The Dana Forum on brain science, 2(4), 50-67.
Teicher, M. H. (2002)
Teicher, M. H. (2002). Scars that Won’t Heal: The Neurobiology of Child Abuse. Scientific American, 286 (3), 68-75.
Provides an in depth overview of research showing that early maltreatment can have enduring and measurable effects on a child’s developing brain, diminishing growth and reducing activity in key areas.
Teicher, M. H., Andersen, S. L., Polcari
Teicher, M. H., Andersen, S. L., Polcari, A., Anderson, C. M., Navalta, C. P., & Kim, D. M. (2003). The neurobiological consequences of early stress and childhood maltreatment. Neuroscience and Biobehavioral Reviews, 27, 33-44.
Abstract
Recent studies have reported an association between exposure to childhood abuse or neglect and alterations in brain structure or function. One limitation of these studies is that they are correlational and do not provide evidence of a cause-effect relationship. Preclinical studies on the effects of exposure to early life stress can demonstrate causality, and can enrich our understanding of the clinical research if we hypothesize that the consequences of early abuse are predominantly mediated through the induction of stress responses. Exposure to early abuse and early stress has each been associated with the emergence of epileptiform electroencephalogram (EEG) abnormalities, alterations in corpus callosum area, and reduced volume or synaptic density of the hippocampus. Further, there is evidence that different brain regions have unique periods when they are maximally sensitive to the effects of early stress. To date, preclinical studies have guided clinical investigations and will continue to provide important insight into studies on molecular mechanisms and gene-environment interactions.
Teicher, M. H., Glod, C. A., Surrey
Teicher, M. H., Glod, C. A., Surrey, J., & Swett, C. (1993). Early childhood abuse and limbic system ratings in adult psychiatric outpatients. Journal of Neuropsychiatry and Clinical Neurosciences, 5(3), 301-6.
Investigated whether early abuse affects the development of the limbic system. The authors hypothesized that intense averse stimulation during early development alters the course of limbic system maturation and results in significant neuropsychiatric sequelae. During initial psychiatric evaluation, 253 outpatients (aged 1769 years) completed the Limbic System Checklist33 (LSCL33) selfreport scale, which was designed to measure somatic, sensory, behavioral, and memory symptoms suggestive of temporal lobe epilepsy. Subjects also completed a questionnaire about physical or sexual abuse. Physical or sexual abuse alone was associated with elevated LSCL33 scores, but only if the abuse occurred before age 18 years. Physical abuse was associated with a 38% increase in LSCL33 scores, sexual abuse with a 49% increase, and combined abuse with a 113% increase. Findings are consistent with a biopsychosocial hypothesis concerning the effects of early abuse on the central nervous system, with these alterations manifesting as persistent behavioral disturbances that are in turn associated with long-term psychiatric sequelae and a proclivity for the intergenerational transfer of abusive and aggressive behavior.
Teicher, M. H., Ito, Y., Glod, C. A
Teicher, M., Samson, J. A., Sheu, Y. S.
Teicher, M., Samson, J. A., Sheu, Y. S., Polcari, A., & McGreenery, C. E. (2010). Hurtful words: Association of exposure to peer verbal abuse with elevated psychiatric symptom scores and corpus callosum abnormalities. American Journal of Psychiatry, 167, 1464-1471.
RESULTS:
Analysis of covariance revealed dose-dependent effects of peer verbal abuse on anxiety, depression, anger-hostility, dissociation, “limbic irritability,” and drug use. Peer and parental verbal abuse were essentially equivalent in effect size on these ratings. Path analysis indicated that peer verbal abuse during the middle school years had the most significant effect on symptom scores. Degree of exposure to peer verbal abuse correlated with increased mean and radial diffusivity and decreased fractional anisotropy in the corpus callosum and the corona radiata.
Terr, L. (1990)
Tomoda, A., Suzuki, H., Rabi
Tomoda, A., Suzuki, H., Rabi, K., Sheu, Y. S., Polcari, A., & Teicher, M. H. (2009). Reduced prefrontal cortical gray matter volume in young adults exposed to harsh corporal punishment. Neuroimage, 47 Suppl 2, T66-71.
Exposing children to harsh CP may have detrimental effects on trajectories of brain development.
U.S. Department of Health and Human Services. (2001)
U.S. Department of Health and Human Services. (2001). In Focus: Understanding the Effects of Maltreatment on Early Brain Development. Washington, D.C.: Government Printing Office.
In 1999, approximately 826,000 children were determined to be victims of abuse and/or neglect (U.S. Department of Health and Human Services, 2001), but it is likely that many more children are actually suffering under adverse conditions. Each one of these children already may have suffered damage to their growing brains. Their brains may be locked into perceiving the world as a cold or dangerous place. They may have great difficulties responding to the caring concern of others. Because their brains’ energies have been focused on survival, on meeting their own needs, these children may not have developed the physical, cognitive, social, and emotional capabilities one would expect of them.
Van der Hart, O., van Dijke, A., van Son
Van der Hart, O., van Dijke, A., van Son, M., & Steele, K. (2000). Somatoform Dissociation in Traumatized World War I Combat Soldiers: A Neglected Clinical Heritage. Journal of Trauma and Dissociation, 1(4), 33-66. (PDF)
Abstract: The massive traumatization of World War I combat soldiers led to an unprecedented number suffering from somatoform dissociative disorders and symptoms, usually diagnosed as hysterical disorders during the war years. Following a brief overview of the scope of the suffering during this Great War, attention is given to British army psychiatrist Charles S. Myers’ (1940) observations of the alternation between a so-called “emotional” personality and an “apparently normal” personality in traumatized combat soldiers. Somatoform dissociation, further categorized into positive and negative symptoms, is related to this structural dissociation, and to fixation in the trauma and avoidance of the trauma, and may be part of a more encompassing symptomatology. Next, a short overview of diagnostic issues is given. We argue that the DSM-IV category of “conversion disorder” is incorrect. Rather the findings revealed here support Janet’s classic and Nijenhuis’ more recent views on somatoform dissociation. Finally, treatment issues are briefly presented.
Van der Kolk, B. A.l (1987)
Van der Kolk, B. A. (1989)
van der Kolk, B. A. (1989). The Compulsion to Repeat the Trauma Re-enactment, Revictimization, and Masochism. Psychiatric Clinics of North America , 12(2), 389-411.
Excerpt “All primates subjected to early abuse and deprivation are vulnerable to engage in violent relationships with peers as adults. Males tend to be hyperagressive, and females fail to protect themselves and their offspring against danger. Chronic physiologic hyperarousal persists, particularly to stimuli reminiscent of the trauma. Later stresses tend to be experienced as somatic states, rather than as specific events that require specific means of coping. Thus victims of trauma may respond to contemporary stimuli as a return of the trauma, without conscious awareness that past injury rather than current stress is the basis of their physiologic emergency responses. Hyperarousal interferes with the ability to make rational assessments and prevents resolution and integration of the trauma. Disturbances in the catecholamine, serotonin, and endogenous opioid systems have been implicated in this persistenence of all-or-nothing responses.”
Van der Kolk, B. A. (1995).
Van der Kolk, B. A. (1995). The body, memory, and the psychobiology of trauma. In Judith L. Alpert (Ed.), Sexual Abuse Recalled: Treating Trauma in the Era of the Recovered Memory Debate. Northvale, NJ: Jason Aronson, pp. 29-60.
This chapter explains amnesia by means of psychobiology. The author provides a brief review of the historical literature on PTSD. Contemporary research on the biology of PTSD indicates that there are persistent and profound alterations in stress hormone secretion and memory processing in people with PTSD. PTSD develops after exposure to intensely distressing events. Extreme stress is accompanied by the release of endogenous neurohormones. Chronic exposure to stress permanently alters how people cope day-to-day and interferes with how they cope with subsequent acute stress. Abnormal psychophysiological responses in PTSD have been observed in response to specific reminders of the trauma and to intense but neutral stimuli, such as unexpected noises. The misinterpretation of unexpected noises as potential threats reflect the inability of people with PTSD to integrate memories of the trauma and their tendency to get mired in a continuous reliving of the past.
Van der Kolk reviews the effect of trauma on the limbic system, which is critically involved in the storage and retrieval of memory. When people are traumatized, the emotional impact of the event may interfere with the capacity of capture the experience in words or symbols. Stress also interferes with hippocampally mediated storage and categorization of memory. Some mental representation of the experience is probably laid down by means of a system that records affective experience but has no capacity for symbolic processing or placement in space or time. It is theorized that the failure of semantic memory leads to the organization of memory on a somatosensory level–such as somatic sensations, behavioral enactments, nightmares, and flashbacks. Research suggests the emotional memory may be indelible but is held in check by cortical and hippocampal inhibitatory control. Decreased inhibitatory control may occur under a variety of circumstances such as under the influence of drugs and alcohol, during sleep, with aging, and after exposure to strong reminders of the traumatic event. Traumatic memories could then emerge as affect states, somatic sensations, or flashbacks. Such somatosensory memories are timeless and unmodified by further experience.
Van der Kolk, B., McFarlane, A., Weisaeth, L. (1996)
Van der Kolk, B. A. (1997)
Van der Kolk, B. A. (1997)
van der Kolk, B. A. (1997). Posttraumatic Stress Disorder and Memory. J Clin Psychiatry, 58(Suppl 9), 16-24.
This review summarizes the current state of our knowledge of the psychobiology of posttraumatic stress disorder (PTSD). People with PTSD develop an enduring vigilance for and sensitivity to environmental threat. They have difficulty in properly evaluating sensory stimuli and responding with appropriate levels of physiologic and neurohormonal arousal. The inappropriate mobilization of biological emergency responses to innocuous stimuli is mirrored psychologically in an inability to properly integrate memories of the trauma and in a fixation on the past. The biological dysregulation of PTSD can be measured on physiologic, neurohormonal, immunologic, and functional neuroanatomical levels. The developmental level at which the trauma occurs affects the nature and extent of psychobiological disruptions. The availability of neuroimaging for documenting structural and functional abnormalities in PTSD has opened up new ways for understanding the neuronal filters concerned with the interpretation of sensory information in PTSD. These studies have produced a number of unexpected findings, which may alter how we conceptualize PTSD and which may force us to reevaluate appropriate therapeutic interventions.
Van der Kolk, B. A. (1997)
van der Kolk, B. A. (1997). Posttraumatic Stress Disorder and Memory, Psychiatric Times, 14(3).
Van der Kolk, B. A. (2002)
van der Kolk, B. A. (2002). In terror’s grip: Healing the ravages of trauma. Cerebrum, 4, 34-50. NY: The Dana Foundation.
Van der Kolk, B. A. (2002)
van der Kolk, B. A. (2002). The Assessment and Treatment of Complex PTSD. In R. Yehuda (Editor) Treating Trauma Survivors with PTSD. Washington, DC: American Psychiatric Press, Inc.
Van der Kolk, B. A., & Fisler. (1995)
van der Kolk, B. A., & Fisler. (1995).Dissociation and the fragmentary nature of traumatic memories: Overview and exploratory study. Journal of Traumatic Stress, 8(4), 505-525.
Abstract: Since trauma is an inescapably stressful event that overwhelms people’s coping mechanisms it is uncertain to what degree the results of laboratory studies of ordinary events have relevance to the understanding of traumatic memories. This paper first reviews the literature on the differences between recollections of stressful and of traumatic events. It then reviews the evidence implicating dissociative processes as the central pathogenic mechanisms that give rise to PTSD. We present the results of a syste matic exploratory study of 46 subjects with PTSD which indicates that traumatic memories are retrieved, at least initially, in the form of dissociated mental imprints of sensory and affective elements of the traumatic experience: as visual, olfactory, aff ective, auditory and kinesthetic experiences. Over time, subjects reported the gradual emergence of a personal narrative that can be properly referred to as “explicit memory”. The implications of these findings for understanding the nature of traumatic me mories is discussed.
Van der Kolk, B. A., Hopper, J. W., & Osterman, J. E. (2001)
van der Kolk, B. A., Hopper, J. W., & Osterman, J. E. (2001). Exploring the Nature of Traumatic Memory: Combining Clinical Knowledge with Laboratory Methods. Journal of Aggression, Maltreatment, & Trauma, 4, 9-31; and Freyd, J. F., & DePrince, A. P. (Editors). Trauma and Cognitive Science (pp. 9-31). Binghamton, NY: Haworth Press.
Van der Kolk, B. A., Pelcovitz, D., Roth, S.
van der Kolk, B. A., Pelcovitz, D., Roth, S., Mandel, F. S., McFarlane, A., & Herman, J. L. (1996). Dissociation, affect dysregulation and somatization: the complex nature of adaptation to trauma. (1996). Dissociation, affect dysregulation and somatization: the complex nature of adaptation to trauma. American Journal of Psychiatry , 153(7 Suppl), 83-93.
OBJECTIVE: A century of clinical research has noted a range of trauma-related psychological problems that are not captured in the DSM-IV framework of posttraumatic stress disorder (PTSD). This study investigated the relationships between exposure to extreme stress, the emergence of PTSD, and symptoms traditionally associated with “hysteria,” which can be understood as problems with stimulus discrimination, self-regulation, and cognitive integration of experience.
METHOD: The DSM-IV field trial for PTSD studied 395 traumatized treatment-seeking subjects and 125 non-treatment-seeking subjects who had also been exposed to traumatic experiences. Data on age at onset, the nature of the trauma, PTSD, dissociation, somatization, and affect dysregulation were collected.
RESULTS: PTSD, dissociation, somatization, and affect dysregulation were highly interrelated. The subjects meeting the criteria for lifetime (but not current) PTSD scored significantly lower on these disorders than those with current PTSD, but significantly higher than those who never had PTSD. Subjects who developed PTSD after interpersonal trauma as adults had significantly fewer symptoms than those with childhood trauma, but significantly more than victims of disasters.
CONCLUSIONS: PTSD, dissociation, somatization, and affect dysregulation represent a spectrum of adaptations to trauma. They often occur together, but traumatized individuals may suffer from various combinations of symptoms over time. In treating these patients, it is critical to attend to the relative contributions of loss of stimulus discrimination, self-regulation, and cognitive integration of experience to overall impairment and provide systematic treatment that addresses both unbidden intrusive recollections and these other symptoms associated with having been overwhelmed by exposure to traumatic experiences.
Van der Kolk, B. A., & Saporta, J. (1991)
Van der Kolk, B. A., & Saporta, J. (1991). The biological mechanisms and treatment of intrusion and numbing. Anxiety Research, 4, 199-212.
Abstract: The recognition that trauma is qualitatively different from stress and results in lasting biological emergency responses following traumatic experiences may account for the biphasic trauma response, and the accompanying memory disturbances. The past decade has seen rapid advances in our understanding of the underlying biology of this “physioneurosis”. In addition to classically conditioned physiological reactions, changes now have been demonstrated in startle response in people with post-traumatic stress disorder and in central nervous system catecholamine, serotonin, and endogenous opioid systems. This paper reviews the research data which have demonstrated changes in these systems and explores how these biological changes may be related to the characteristic hyper-reactivity, loss of neuromodulation, numbing of responsiveness, dissociative states, and memory disturbances seen in PTSD. There is growing evidence that trauma has different biological effects at different stages of primate human, development. This article relates these findings to the studies which have demonstrated clear linkages between childhood trauma, and a variety of psychiatric disorders, including borderline personality disorder, and a range of self-destructive behaviors.
Van der Kolk, B. A., Van der Hart, O., & Burbridge, J.(1995)
Van der Kolk, B. A., Van der Hart, O., & Burbridge, J.(1995). Approaches to the Treatment of PTSD. in S. Hobfoll & M. de Vries (Eds.), Extreme stress and communities: Impact and intervention (NATO Asi Series. Series D, Behavioural and Social Sciences, Vol 80). Norwell, MA: Kluwer Academic.
This article considers PTSD as a biological disorder, and discusses the roles of developmental level, memory, and dissociation in its formation. Bessel van der Kolk and his colleagues review the symptomatology of PTSD in detail, and describe three principle components of treatment, before turning to specific tasks guiding psychotherapeutic interventions including group therapy and psychopharmacological approaches. Two Tables summarize symptoms of simple PTSD and additional features associated with the proposed diagnosis of complicated PTSD. Includes about 70 references.
Vermetten, E., Schmahl, C., Lindner, S., Loewenstein, R. J., & Bremner, J. D. (2006)
Vermetten, E., Schmahl, C., Lindner, S., Loewenstein, R. J., & Bremner, J. D. (2006). Hippocampal and amygdalar volumes in Dissociative Identity Disorder. American Journal of Psychiatry, 163, 630-636.
The authors used magnetic resonance imaging to measure the volumes of the hippocampus and amygdala in 15 female patients with dissociative identity disorder and 23 female subjects without dissociative identity disorder or any other psychiatric disorder. The volumetric measurements for the two groups were compared. Hippocampal volume was 19.2% smaller and amygdalar volume was 31.6% smaller in the patients with dissociative identity disorder, compared to the healthy subjects.
Reprints: e.vermetten@umcutrecht.nl
